
Osteochondrosis is a form of degenerative disease of the joints and intervertebral discs. Osteochondrosis affects the cartilaginous tissue of the discs. As a result, the disc hardens and shrinks, losing cushioning properties and causing severe pain.

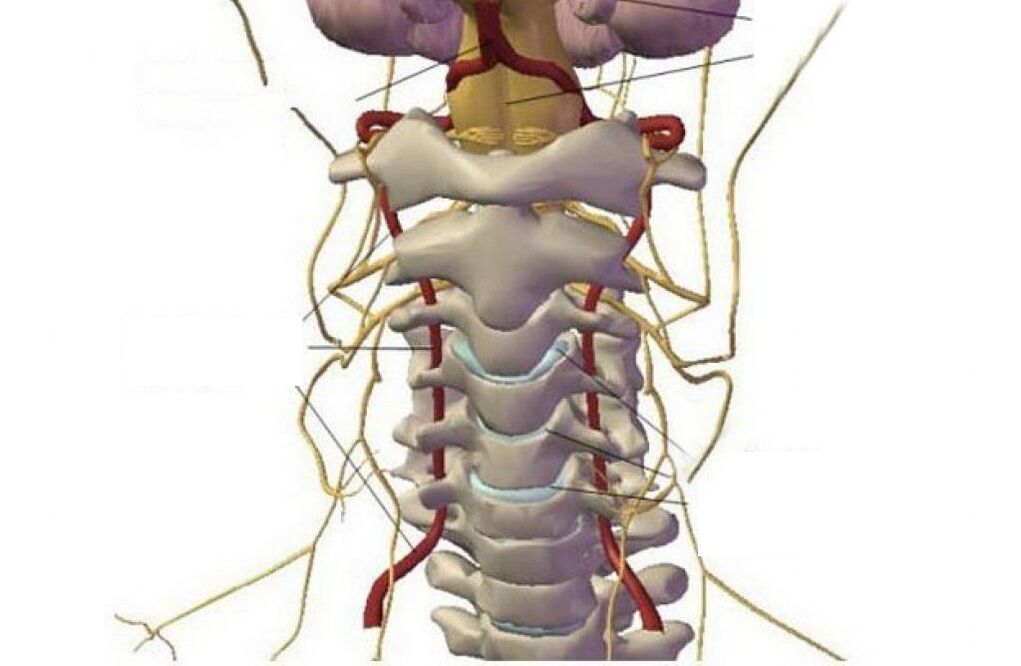
Cervical osteochondrosis is a progressive degenerative-dystrophic process that leads to the depletion, deformation and destruction of the intervertebral discs in the cervical region. Loss of shock-absorbing cartilage causes pain both by exposing the joint surfaces (spondyloarthrosis) and by compressing the nerve roots of the spinal cord.
In the absence of timely treatment, ossification of the spine is possible with loss of its natural flexibility, impaired blood supply to the brain, deterioration of nerve conduction in the parts of the body that innervate the roots of the cervical spine.
The pathology can develop either independently or as part of a general spinal injury, covering the thoracic, lumbar, and sacral regions.
General information about cervical osteochondrosis
Osteochondrosis of the cervical spine is believed to be more common than in other departments. In fact, this is not so - dystrophic phenomena develop evenly at all points of maximum load - in the area of the main curves of the spine (the lower the department is located, the greater the load it bears). However, the symptoms of cervical osteochondrosis are more pronounced, so they seem to be a more frequent occurrence. This is due to the high mobility of the neck vertebrae, which at the same time hold the head, as well as the peculiarity of the location of the exits of the roots of the spinal cord.
On a note!According to statistics, the disease affects more than 60% of middle-aged and elderly people. However, recently there has been a rejuvenation of the pathological process - pathology occurs in young people and even in teenagers. This is due to the general computerization of study and work, as well as a decrease in physical activity and a deterioration in the quality of nutrition.
Taking into account the age group, 2 forms of cervical osteochondrosis can be distinguished - physiological and pathological.
physiological processassociated with the natural aging of the body, when the symptoms of the disease are a consequence of the gradual wear of the intervertebral discs. The process occurs under the influence of the endocrine system and is a consequence of menopausal changes. Destruction of cartilage structures starts from the center of the intervertebral disc and is accompanied by a gradual replacement of cartilaginous tissue by fibrous tissue. The pathology is irreversible, but it can be compensated by special drugs.
pathological processassociated with abnormal destructive changes in the body - immune, dystrophic, inflammatory, metabolic. Firstly, pericartilaginous tissues are involved - salt deposits appear in bone structures, nerve roots become inflamed, atrophy or hypertonicity of skeletal muscles occurs, which leads to impaired blood circulation in the head-neck-chest region. With timely diagnosis, the pathology is treatable and ends with the complete restoration of healthy organ and tissue function.
Stages of cervical osteochondrosis and its symptoms
There are 4 main stages of the pathological process:
- Stage 1 - is expressed by slight discomfort and muscle tension in the diseased area, cartilage discs lose their stability;
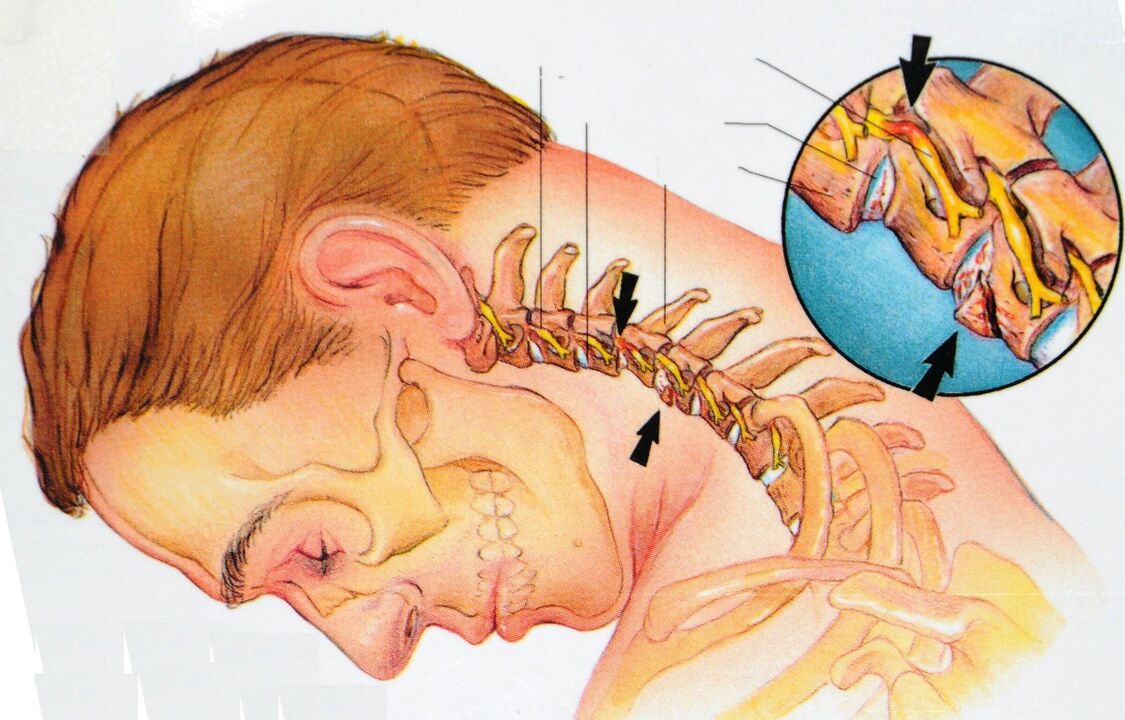
- Stage 2 - there is local pain, especially when moving the head. Intervertebral discs are deformed, the annulus fibrosus begins to collapse, the distance between the vertebrae is reduced;
- Stage 3 - Pain intensifies and becomes constant, movements are limited. Turning the head can provoke bouts of dizziness, nausea, impaired blood supply to the brain leads to general lethargy, fatigue, impaired concentration, cartilage becomes thinner, vertebrae close, annulus fibrosus is completely destroyed with risk of intervertebral hernia ;
- 4th stage - the pain syndrome completely immobilizes the neck region; blood circulation to the brain is impaired and requires constant medical support; the vertebrae begin to grow together.
Cervical osteochondrosis: signs, symptoms, treatment of the pathology
In the early stages, osteochondrosis is asymptomatic. As the disease develops, a distinguishing feature becomes the presence of painful or uncomfortable sensations in the head, neck, and chest, less often in the upper limbs.
All possible symptoms can be conditionally attributed to 4 types of syndromes: cardiac, vertebral, radicular (nervous) and vertebral artery syndrome (with circulatory disorders).
Vertebral Syndrome:
- neck crunch when turning/tilting head;
- as the disease progresses, pain and difficulty in movement occur;
- morphological structural disorders in the vertebral body and intervertebral space (visible on x-rays).
heart syndrome:
- shortness of breath, weakness;
- feeling of incomplete inspiration, shortness of breath;
- spontaneous phenomena of the cardiovascular system - angina pectoris, retrosternal pain, burning;
radicular syndrome:
- numbness of tongue, shoulders, fingers, occipital region;
- difficulty swallowing;
- discomfort in the area between the shoulder blades;
- headache in the occiput and forehead.
vertebral artery syndrome:
- irrational jumps in blood pressure;
- dizziness, even loss of consciousness;
- tinnitus, cotton sensation in the head;
- temporary unilateral blindness, "flies" in the eyes;
- periodic bouts of nausea, especially when moving the head;
- headaches - mostly in the back of the head, as well as migraines;
- drowsiness, decreased performance, memory, concentration, depression.
Heads up!All these syndromes must be combined with each other. The absence of symptoms of one of them may be a reason for differential diagnosis with other groups of diseases.
Causes of cervical osteochondrosis
Dystrophic phenomena in the cervical spine region are associated with the vertical position of the skeleton and the specific distribution of static and dynamic loads, which largely depend on the prevailing posture and the degree of development of the skeletal muscles.
- lack of movement - which does not develop - degrades: muscles weaken, tissues are destroyed;
- incorrect static postures - muscle clamps lead to circulatory disorders with subsequent tissue degeneration;
- lack of nutrition or an unbalanced diet - the body must receive everything necessary for the construction and renewal of bone and cartilaginous structures of the skeleton, maintaining muscle tone;
- obesity, overweight, carrying heavy loads - the load on skeletal structures increases;
- constant nervous tension and nervous stress;
- hypothermia of the cervical region - "cold", "swollen" - provokes hidden inflammatory processes;
- the presence of autoimmune diseases involving cartilage leads to its premature destruction;
- endocrine pathologies interrupt mineral metabolism, reduce the absorption of calcium, silicon, phosphorus and other elements of bone and cartilage tissue;
- neck injuries;
- Congenital anomalies of the spine and adjacent muscles.
Diagnosis of cervical osteochondrosis

The diagnosis of "osteochondrosis of the cervical vertebra" is made difficult by the low specificity of the symptoms and the wide variety of its manifestations. During the examination, you will need to consult a neurologist, surgeon, orthopedist, cardiologist.
A physical examination is performed by a physician with a questioning of the patient. The main diagnostic burden is on instrumental and laboratory research methods.
- radiography of the cervical region; in the initial phase of the process, MRI of the cervical region will be more informative - it will provide high-quality visualization of hard and soft tissues - it will show the condition of the intervertebral discs, the presence of osteophytes, deformities, damage to the nerve roots and blood vessels; assess the condition of ligaments, muscles, bone tissue; shows the dynamic state of soft tissues;
- Dopplerography of the neck vessels will help to assess hemodynamics and the degree of damage to blood vessels (in particular, the state of the vertebral artery);
- contrast myelography - will help in the suspicion of violation of nervous processes;
- ECG and echocardiography of the heart are used in the differential diagnosis of cardiac syndrome with cardiovascular diseases.
How to treat cervical osteochondrosis
A complex of therapeutic measures is formed taking into account the stage of the disease (acute, chronic), the degree of damage and the causes of the pathology. Use conservative treatment, surgery, a mixed approach.
conservative impact
It is a gradual restoration or compensation of damage in the context of symptomatic treatment. It includes drug therapy, physical therapy, exercise therapy and massage methods.
Medical treatment:
- analgesics - mainly topical gels and ointments; in severe cases - general analgesics in the form of tablets;
- anti-inflammatory drugs - NSAIDs, as well as corticosteroids (short course if necessary);
- drugs to improve microcirculation and blood circulation in general;
- chondroprotectors - means to protect and restore cartilage tissue;
- muscle relaxants - to eliminate muscle cramps and spasms;
- complexes of vitamins and microelements - necessary for nutrition and support of tissues with building elements.
As the acute symptoms subside, physiotherapy, exercise therapy and self-massage methods are connected.
Physiotherapyimproves the nutrition of cartilaginous and bone tissues, due to the restoration of blood supply to the damaged area. To avoid complications, it is recommended to use the method of isometric movements, when instead of real turns and tilts of the head, which can cause damage, its imitation is used.
Heads up!All actions should be carried out only after diagnosis and consultation with a doctor.
The technique allows you to develop and strengthen the short atrophied muscles of the neck and stabilize the position of the cervical spine. The sequence of basic exercises:
- Place the palm of the right hand on the side of the head - for 10 seconds, press the palm of the hand to the head, while tensing the muscles of the head and neck for resistance - the head must remain still.
- Lower your hand, relax your head and neck muscles as much as possible for 20 seconds.
- Repeat the exercise with your left hand.
- Place both hands on your forehead with your palms - for 10 seconds, press your forehead, as if trying to tilt your head back, while tensing your neck muscles to resist the movement. The head must remain still.
- Lower your arms, relaxing the muscles as much as possible, similar to the previous exercise.
- Place both palms of your hands on the area above the back of your head. By analogy, perform a pressure load on the neck muscles, trying to tilt the head forward - it should still be still.
- Lower your arms, relax your neck and head muscles. Repeat the exercise set 4-10 times.
After strengthening the short neck muscles, you can start performing dynamic exercises.
On a note!Swimming and water aerobics proved to be a technique to restore cervical mobility.
self massageallows to reduce the intensity of local reactions and relieve muscle cramps during static work. Execution rules:
- area of influence - the back of the head, the back and the side surfaces of the neck;
- perform the procedure in a sitting position;
- the movements must be carried out in the direction of the spine;
- use only your fingertips;
- avoid pressure on inflamed areas;
- perform movements smoothly - sharp pressure can harm.
Physiotherapytypical for hospital treatment and spa rehabilitation. Well proven:
- electrophoresis - warms the area, improves microcirculation, is used for deeper penetration of topical preparations;
- magnetotherapy;
- amplipulse;
- UHF.
Surgical intervention is indicated for complicated extrusion, spinal cord violation, and intractable pain syndromes.
What is dangerous cervical osteochondrosis
The neck area concentrates a dense intertwining of the main blood vessels, nervous processes and dynamic structures of the bony skeleton. In the absence of treatment, serious pathological changes can be observed:
- weakening of the annulus fibrosus causes dislocations and subluxations in the area of the most mobile vertebrae;
- the presence of osteophytes and muscle spasm leads to the violation of nerve roots and blood vessels with the formation of compression syndromes;
- destruction of cartilaginous discs and convergence of vertebrae leads to intervertebral hernias with violation of nervous tissue.
Each of these phenomena is followed by a pronounced negative reaction of the whole organism.
Possible complications and consequences
The list of the most common complications of cervical osteochondrosis includes:
- vegetovascular dystonia;
- hypertension;
- lack of oxygen to the brain and its structures;
- retinal dystrophy of the visually impaired eye;
- malfunction of the thyroid gland;
- esophageal and tracheal dysfunction - difficulty swallowing and respiratory spasms;
- intractable pain in the head, neck, chest, upper limbs;
- convulsions and numbness of the face, hands;
- disruption of the hypothalamic-pituitary system, which leads to the failure of all hormonal activity in the body.
Preventive measures of cervical osteochondrosis
The most effective treatment is disease prevention. Prevention will help you with this. Just follow some basic recommendations:
- correct your posture,
- create a comfortable workplace;
- during sedentary work, take breaks for a "minute of physical education";
- include in your diet foods rich in calcium, magnesium, phosphorus, silicon - fish, nuts, seeds, legumes, dairy products, fresh vegetables, fruits; limit the intake of salty, sweet, starchy and spicy foods;
- to sleep and rest, use an orthopedic mattress and pillow;
- practice a sport without strength - it is better to give preference to swimming.
Even if you can't take into account all the requirements, moderate exercise, proper nutrition and attention to your posture can significantly reduce your risk of developing pathology.
The hidden cause of impotence, male and female infertility is osteochondrosis
Even at school, in biology classes, they tried to convey important information about the huge role of the spine in maintaining human health. Unfortunately, many then were engaged in more important things and did not listen to the words of the teachers. But in vain! Doctors say that disorders of the musculoskeletal system, in particular, caused by osteochondrosis, can cause the development of a large number of various serious diseases.
Why osteochondrosis has a powerful destructive effect on the human body
Often men suffer from impotence and infertility, and women try in vain to get pregnant and do not even suspect that this can be caused by common osteochondrosis. The fact is that the cause of the development of the disease lies in the violation of the blood supply to the tissues of the vertebrae and the muscles that surround them. As there are no blood vessels in the intervertebral discs, they are the first to suffer from a lack of water and various other substances. This leads to cartilage cracking, which means the discs are no longer able to absorb the load on the spine. This is where the constant back pain comes from.
If at this stage you do not intervene in the process, then osteochondrosis will continue to progress and cause complications, for example, a herniated disc. This, in turn, causes a violation in the segmental apparatus of the spinal cord and impairs blood circulation, including in Organs pelvic organs. This is the main reason for the development of many disorders in the work of internal organs, as well as impotence and infertility of interest to us.
The development of impotence in men, in addition to violations at the physical level, also contributes to the psychological factor. After all, for every normal, well-rounded man, even a single failure in bed becomes drama, and it doesn't matter if it's caused by an exacerbation of osteochondrosis, sciatica, or other sources of back pain.
Men may begin to experience erection difficulties in the presence of cervical or lumbar degenerative disc disease. But in each case, the pathology develops according to its own mechanism.
cervical osteochondrosis
In the presence of this type of disease, there is a decrease in the quality of blood circulation in the brain, which causes dysfunctions in the production of sex hormones and substances responsible for vascular tone. Therefore, with cervical osteochondrosis, most often patients complain of decreased sexual desire, anorgasmia and problems with ejaculation.
lumbar osteochondrosis
Since the pelvic area, i. e. here the male genitals are located, is, so to speak, in a "turned off" state due to disorders in the spinal cord, nerve impulses do not always manage to reach the genitals, which leads to to erectile dysfunction.
Female and male infertility as a result of osteochondrosis
Often, in the absence of other prerequisites, unsuccessful attempts to conceive a child in both men and women can be the result of pathological processes that accompany osteochondrosis. Most often, the cause of the problem lies not so much in the violation of the blood supply to the organs located in the small pelvis, but in neurological disorders.
Exams of women suffering from infertility show degenerative changes in the lower thoracic spine and lower back. In infertile men, osteochondrosis affects the lumbosacral region. Such differences in the areas affected by osteochondrosis are explained by the peculiarities of the structure and innervation of Organs pelvic organs in representatives of different sexes.
Sometimes women cannot get pregnant, even if they don't show any signs of the disease and don't feel the slightest discomfort in their back. This is mainly due to the fact that disorders in the reproductive system can occur even if only the anterior roots of the spinal cord are damaged, which is not accompanied by pain.
Therefore, everyone who suffers from disorders of sexual and reproductive functions is strongly recommended to undergo the most thorough examination of the body, not forgetting the neuropathologist and vertebrologist. It is possible that the root of the problem lies precisely in the pathologies of the spine.
































