Osteoarthritis is the collective name dystrophic-degenerative diseases of the articular apparatus of different localization and etiology with similar clinical and morphological picture and the outcome and manifested by lesions of the articular cartilage, subchondral bone formation, capsules, ligaments.

Osteoarthritis is the most common pathology in rheumatology practice, according to medical statistics, suffer them to 1/5 of the total population. Osteoarthritis is a significant cause of reduced quality of life in approximately half of patients, most of whom become disabled. The incidence depends on the age: osteoarthritis is rare in young age, debuting most often after 40-45 years, with individuals older than 70 years radiographic signs are defined in the vast majority of cases. At the young age of incidence of approximately 6.5%, after 45 years – 14-15%, after 50 years – 27-30%, and individuals older than 70 years is 80 to 90%.
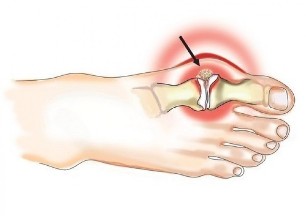
Most often arthritis in the pathological process involved the small joints of the hand (women 10 times more often than men), the big toe, the intervertebral joints of the thoracic and cervical spine and the knee and hip joints. Osteoarthritis of the knee and hip joints leads in severity of clinical manifestations and negative impact on quality of life.
For osteoarthritis is characterized by complex lesions of the articular and auxiliary devices:
- inflammatory changes of the cartilage of the joint;
- the involvement in the pathological process be of bone structures;
- synovitis – inflammation of the inner lining of the joint capsule;
- bursitis – the defeat of bags around the joints;
- reactive inflammation of the soft tissues (muscles, subcutaneous tissue, ligaments), which are located in the projection of the involved joint.
Since the root cause of osteoarthritis is inflammatory changes, in some Western countries is called a disease arthritis. In Russian medicine, the terms arthritis and osteoarthritis occur equally often and involve the same pathological process. Recently in rheumatology practice, the most often used term for osteoarthritis, emphasizing the involvement in the pathological process in the joint as a movable connection, but also the underlying bony structures.
The consequences of arthrosis in the absence of adequate treatment, become a progressive decrease in range of motion in the affected joint, immobilization.
Currently, the approach to the understanding of osteoarthritis has changed dramatically: the disease is regarded as an aggressive process of destruction of cartilage tissue under the influence of inflammation, which requires mandatory active anti-inflammatory therapy.
Synonyms: arthritis, osteoarthritis, osteoarthritis, deforming osteoarthritis.
Causes and risk factors
In the scientific community debate about the root causes of joint damage. Some researchers assign a major role to damage of cartilage covering the articular surfaces under the influence of various factors that leads to the violation of the biomechanics of the joint and degenerative changes of the surrounding structures. Others, however, see the root cause in the defeat of the surface layer of articulated bone structures forming the joint (for example, due to microcirculatory disturbances) and secondary changes think dystrophy and degeneration of cartilage.
The causal factors that most frequently provoke the development of osteoarthritis:
- prior acute traumatic injury of the joint (rupture or tearing of the ligaments, contusion, dislocation, intra-articular fracture, penetrating trauma);
- systematic excessive load associated with a particular activity (professional athletes, dancers, individuals involved in heavy physical labour, etc.);
- obesity;
- local influence of low temperatures;
- chronic disease in which affect the local circulation (endocrine pathology, pathology of the vascular bed, etc.);
- acute infectious diseases;
- hormonal changes (pregnancy, menopause);
- autoimmune diseases involving connective tissue damage;
- connective tissue dysplasia (congenital weakness of this type of tissue, accompanied by increased mobility of joints);
- genetic abnormality – genetic defect, which is localized on chromosome 12 and encoding procollagen type II (COL2A1) or VDR gene which controls vitamin D-endocrine system;
- congenital structural and functional abnormalities of the articular apparatus;
- Mature, elderly and senile age;
- bone thinning (osteoporosis);
- chronic intoxication (including alcohol);
- moved surgery on the joints.
In most cases, arthrosis is of poly-etiological nature, i.e. it evolves under the combined influence of several causal factors.
The symptoms of osteoarthritis
For osteoarthritis is not characterized by acute clinical picture, changes in the joints are progressive, slow growing character that is manifested by a gradual increase in symptoms:
- pain;
- intermittent crunch in the affected joint;
- deformity of the joint, appearing and increasing as the disease;
- stiffness;
- the limitation (reduction of the volume of active and passive movements in the affected joint).
Pain in osteoarthritis is stupid transient nature, appears in the movement, amid a heavy load, the end of the day (may be so intense that it allows the patient to sleep). Continuous non-mechanical nature of pain for osteoarthritis are uncommon and indicates the presence of active inflammation (subchondral bone, synovial membrane, ligaments, or periarticular muscles).
The majority of patients said the presence of so-called starting pain that occurs in the morning upon waking or after a long period of inactivity and passing during physical activity. Many patients define this condition as the need "to develop a joint" or "separate."
For osteoarthritis characteristic morning stiffness that is well localized and is of short duration (no more than 30 minutes), sometimes it is perceived by patients as "feeling jelly" in the joints. You may have a feeling of jamming, stiffness.
With the development of reactive synovitis the symptoms of osteoarthritis join:
- tenderness and local rise in temperature, which is determined by palpation of the affected joint;
- the constant character of the pain;
- the increase in joint volume, swelling of soft tissues;
- a progressive decrease in range of motion.
For osteoarthritis there is an increase in joint volume, swelling of soft tissues.

Diagnosis
Diagnosis of osteoarthritis is based on the assessment of anamnestic data, the characteristic manifestations of the disease, results of instrumental methods. Changes in General and biochemical blood tests for osteoarthritis are not characteristic, they appear only in the development of an active inflammatory process.
The main instrumental method of diagnosis of osteoarthritis is x-ray, in diagnostically unclear cases recommended to conduct the CT or magnetic resonance imaging.
Osteoarthritis of the knee and hip joints leads in severity of clinical manifestations and negative impact on quality of life.
Additional diagnostic methods:
- arthroscopy;
- ultrasonography (evaluation of the thickness of the articular cartilage, synovial membrane, articular condition handbags, the presence of the liquid);
- scintigraphy (assessment of the status of bone tissue of the heads of the bones forming the joint).
Treatment of osteoarthritis
Drug therapy:
- non-steroidal anti – inflammatory drugs- the relief of pain and signs of inflammation during exacerbation;
- glucocorticosteroid hormones intra-articular injection for relief of synovitis phenomena; apply limited, in cases where it is necessary in the shortest possible time to eliminate the painful symptoms;
- antifermental drugs (proteolysis inhibitors) – prevent the progression of dystrophic and degenerative processes in cartilage and bone tissue;
- antispasmodics – eliminate local muscle spasm in the damaged segment;
- anabolic medications speed up the regeneration of damaged tissue;
- the drugs directed on correction of the properties of the blood, strengthening vascular walls, increase their elasticity and tissue regeneration – help to strengthen the walls of microcirculatory vessels, ensuring adequate blood supply to the damaged area;
- means of improving microcirculation;
- medications for arthritis – despite their massive distribution in the treatment of arthritis, a wide placebo-controlled studies the clinical efficacy of this group of drugs has not been proven.
Physiotherapy techniques used for the treatment of osteoarthritis:
- massage regional muscles, improve circulation and relieve local spasm;
- active kinesiotherapy, i.e. exercising with osteoarthritis with the use of special equipment;
- therapeutic exercises for osteoarthritis;
- laser therapy;
- ultrasonic treatment;
- therapeutic baths, mud and paraffin; etc.
With the ineffectiveness of these methods of influence, in the presence of complications resort to surgical treatment of osteoarthritis:
- the decompression of meta-and epiphysis of the bone inside the prolonged blockade (reduction in intraosseous pressure in the affected area);
- corrective osteotomy;
- replacement of joints.
In the early stages of the disease are used mechanical, laser device (smoothing the surface of damaged cartilage, removal of non-viable plots). This method effectively relieves the pain, but is temporary in effect – 2-3 years.

Possible complications and consequences
The effects of osteoarthritis, especially in the absence of adequate treatment, are:
- a progressive decrease in range of motion in the affected joint;
- immobilization.
Forecast
Forecast favorable for life. A favorable social and labor prognosis depends on timeliness of diagnosis and treatment, reduced when delaying the decision on the surgical treatment of the disease if necessary.
Prevention
- The rejection of heavy loads, prolonged static tension of the affected joint.
- Wearing the orthoses if necessary.
- Diet for osteoarthritis, aimed at reducing body mass.
- Prevention of hypothermia.
- Proper treatment of acute injury of the joints to full recovery with mandatory rehabilitation.
- Clinical monitoring for symptoms of osteoarthritis.
































