Osteochondrosis is a degenerative-dystrophic disease of the cartilage structures of the spine, which leads to a violation of the structure and the functional properties of the intervertebral discs and the surrounding musculoskeletal system. There are three main types of osteochondrosis, depending on the location:

- cervical;
- chest;
- lumbar.
According to statistics from the World Health Organization, 50% to 90% of the world population is affected by this disease. It should be noted that osteochondrosis is rapidly becoming younger in recent years. Today, on a detailed examination, it will be difficult to find a person over 20 years of age without protruding discs and other primary signs of this disease, and the average age for the appearance of full clinical signs (chronic pain, postural disorders, etc. ) is 30-36 yearsxx / p>
causes of osteochondrosis
The main causes of osteochondrosis of the spine are:
- sedentary lifestyle;
- hereditary predisposition;
- Metabolic and gastrointestinal disorders that interfere with the normal absorption of essential nutrients by the body;
- Occupational risks, mostly exposed to vibrations;
- Development of scoliosis and various types of postural disorders during the active growth of the body;
- insufficient water absorption, permanent dehydration;
- Metabolic disorders, malnutrition and lack of essential nutrients in the diet;
- violation of calcium metabolism in the body;
- increased physical activity and traumatic sports;
- uncomfortable shoes;
- chronic stress;
- trauma;
- congenital abnormalities in the development of the musculoskeletal system.
Most of the time this is the fault of the lifestyle most modern people lead and the nature of the disease. Osteochondrosis is called a person's payment for walking upright.
Unfortunately, nature has not yet developed a reliable protective mechanism against the negative effects of vertical pressure. When running, jumping and other assembly loads, our discs contract and expand under the influence of the vortices, acting as shock absorbers. In such a situation, the cartilage tissue is subjected to constant microtraumatisation. Gradually there are more such microtraumas, and if at a young age the body's reserves are sufficient to mend and restore them, after 21 years these processes are greatly inhibited, and from 25 years they completely decrease, and the processes of degeneration outweigh the processes of regeneration.
Due to a lack of exercise, uncomfortable sitting postures, bad habits, lack of sleep, insufficient rest, stress, the work of the blood vessels deteriorates, less nutrients flow and the nutritional processes of the intervertebral discs are disturbed. This eventually leads to the cartilage wearing out.
Genetic predisposition also plays an important role in the rate of development of osteochondrosis. One of the main factors in the progression of the disease is deviations in the synthesis of connective tissue. Sometimes these errors appear in the course of life and are caused by lifestyle and age factors, but more often it is our genes to blame.
Exactly the likelihood of the disease can also depend on how susceptible, at the genetic level, various diseases and other structures of the human body are, on which the work and nutrition of the entire spine depends.
Mechanism of the development of osteochondrosis
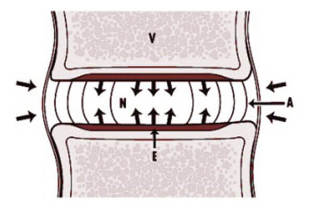
The intervertebral disc is an elastic gelatinous body. Like any cartilage tissue, it contains special substances - mucopolysaccharides. During physical activity, the metabolism in the body of the disc increases and more nutrients flow into the disc. The number of incoming enzymes increases, which changes the properties of mucopolysaccharides. They attract more water from the intercellular space, the intervertebral disc swells and balances the load on the vertebrae. The process of binding water continues until the pressure on the disc comes into equilibrium. When the load is removed, the process is reversed. The water returns, the elasticity of the disc body decreases and the dynamic equilibrium is restored.

In the case of osteochondrosis, changes occur in the body of the intervertebral disc. The amount and composition of the mucopolysaccharides changes, the content of chondroitin sulfates and hyaluronic acid can decrease. As a result, all of this leads to dehydration of the nucleus pulposus. The disk loses its elasticity, decreases in volume and can normally no longer withstand the load acting on it. The nucleus pulposus also begins to lose elasticity.
The changes that occur lead to a violation of the shock-absorbing properties of the pane, which has a negative effect on its ability to be fixed. With movement or exertion, some parts of the spine can move, albeit slightly, relative to each other. A weakened fixation can initially be compensated for by the strength of the muscles and ligaments. However, in the future, under the influence of various negative factors (prolonged stay in a fixed vertical position, postural disorders, intense physical exertion), pathological changes or atrophy of the muscular-ligamentous apparatus may occur. The reverse process can also occur - an excessive increase in muscle fixation. The muscle groups that are responsible for the fixation of the spine become too tense, and this condition does not go away even at rest.
Due to uneven load distribution, sprains, muscle weakness, progressive degenerative changes in the intervertebral discs, changes occur in the bone tissue of the surrounding vertebrae. The density of the bone structures begins to increase as the body begins to pump calcium there to compensate for the pressure that the disc previously exerted on itself during exercise.
diagnosis of osteochondrosis
The primary diagnosis is made based on the patient's complaints and preliminary examination. Under rest and movement conditions, it is checked whether there is pain in different parts of the spine. The doctor determines the localization of the pain, its duration, specifies the factors that provoke the pain. In these cases the pain intensifies and decreases. It indicates how long the disease lasted, what contributed to its onset, how it progressed, under what circumstances an exacerbation occurs, and how the patient feels during remission.
Next, the degree of the spinal lesion is determined. The possible range of motion is set:
- tilted (forwards, backwards, sideways);
- Rotational movements in different parts of the spine.
It is necessary to pay attention to the physiological curves of the spine and the possible flattening (in rare cases, reinforcement) of the lordosis in the lumbosacral and cervical areas. Possible presence of possible deformities of the spine is determined:
- scoliosis;
- involuntary tilting of the head to the painful side;
- inclined pelvic position.
Possible violations of the sensitivity are determined. The condition of the muscle-ligament apparatus is assessed, a possible decrease in tone and muscle atrophy.
X-ray

The condition of the affected vertebrae and intervertebral discs can be assessed with the X-ray examination. The image can be recorded in two mutually perpendicular planes - straight and to the side as well as in two inclined projections. X-rays are taken while standing or lying down. If necessary, the X-ray can be taken in the flexion-extension position and tilted to the side.
MRI (MAGNETIC RESONANCE TOMOGRAPHY)
The most informative method of diagnosing osteochondrosis. In addition to the bone structures, the condition of the soft tissues surrounding the spine (cartilage, blood vessels, muscles, ligaments, nerves, etc. ) can also be assessed. The MRI can be performed in three projections. In contrast to tomography, the body is not exposed to X-rays.
CT (COMPUTER TOMOGRAPHY)
Has several advantages over the X-ray examination. X-rays show better changes in the bone structures of the vertebrae, the height of the intervertebral disc, the osteophytes that develop, and bone growth, as well as the presence of subchondral sclerosis. However, with CT you can identify possible disc ruptures, compression of the roots and changes in the dura mater of the bone marrow
ELECTROMYOGRAPHY (EMG)
EMG is an evaluation of the bioelectrical potentials of the spinal muscles that arise when aroused. In fact, it is a method of recording the electrical activity of muscle fibers. Promotes a more objective diagnosis of osteochondrosis as well as control over the course and prognosis of the disease.
RHEOGRAPHY
Is used to examine the condition of the vessels of the extremities, the brain and the back in the case of lesions in certain parts of the spine.

Rheovasography (RVG) is a type of rheography that is performed when examining the vessels of the arms and legs. With radicular syndrome, spastic phenomena appear in the arteries of the upper and lower extremities, mainly from the side of the lesion. You can identify them with RVG.
Rheography is particularly informative for various vascular events in the affected area of the spine, especially in the syndrome of a compressed artery. This research method allows you to indirectly assess the condition of the affected vertebra and track the dynamics of the disease.
ELECTROENCE PHALOGRAPHY (EEG)
Investigation of the biopotentials of the brain in osteochondrosis of the cervical spine. The EEG is most informative when performing head rotation and neck lengthening tests. Allows the detection of abnormalities in the vertebral arteries that lead to an interruption in the blood supply to the brain. The study evaluates the rhythm, frequency and amplitude of waves. Arterial lesions are manifested by flattening and desynchronization of the encephalogram. In severe cases, the rhythm may be poorly expressed or absent. There can also be a number of other pathological phenomena that a specialist can decipher.
Treatment of osteochondrosis
Treating diseases always requires an integrated approach. Depending on the severity and severity of the manifestations, the course of intensive therapy can last 1 to 3 months, and additional prophylaxis can be carried out to consolidate the result achieved for up to 1 year.
The treatment can be carried out in two directions: conservative and operative.
CONSERVATIVE TREATMENT FOR OSTEOCHONDROSIS
This type of therapy aims to relieve pain, increase the healthy range of motion of the spine, and prevent the further development of the disease. Contains the following instructions:
- drug therapy;
- Physiotherapy;
- movement therapy (physiotherapy exercises);
- massage;
- Manual therapy;
- osteopathy;
- Innovative techniques (stem cells);
- Psychological rehabilitation;
MEDICAL THERAPY
If the pain syndrome is pronounced and the quality of life deteriorates significantly, the use of a nerve block is recommended. Blockages are divided into the following types:
- Blocking of the trigger points (muscle seals due to uneven distribution of the load on the back muscles);
- Intraosseous - injection of an anesthetic into the corpus spongiosum for pain relief and treatment of accompanying neuralgic, motor and vascular disorders;
- facet - injection of an anesthetic to relieve pain in nerve roots and facet joints;
- Paravertebral - the introduction of drugs into the spine in the places where the nerve roots emerge to temporarily disable the pain reflex;
- epidural - injection of a drug into the epidural space of the lumbosacral spine with radicular syndrome to relieve pain;
Groups of medicinal products for the treatment of osteochondrosis:
- Anti-inflammatory drugs - are used to stop inflammatory processes;
- antispasmodics - to relieve cramps;
- antioxidants - to prevent the effects of free radicals that accelerate aging and the development of degenerative processes in tissues;
- Preparations to improve blood circulation in the spine;
- Chondroprotectors - for the regeneration and inhibition of the degeneration processes of the cartilage tissue.
Chondroprotectors are an essential part of the therapeutic treatment of osteochondrosis. They are available in three forms: injectable, tablet, and ointments and creams.
Medicines can be prescribed for external use in the form of ointments and gels, for intramuscular injection in the form of injections, and orally in the form of capsules and tablets.
Medicines are only prescribed by a doctor. In the absence of pain and pronounced degenerative changes, the use of drugs is not justified. Treatment of osteochondrosis is impossible with the help of drugs alone. Therapy should include diet, optimal physical activity, physical therapy, if possible, psychological rehabilitation, and other preventive measures.
MASSAGE TO PREVENT OSTEOCHONDROSIS
The advantages of massage are as follows:
- Improvement of the blood circulation, stabilization of the metabolic processes of the intervertebral disc and the surrounding tissue;
- Removal of muscle-ligament spasms;
- Strengthening of the muscles and relief of the spine;
- Inhibition and prevention of the development of inflammatory processes;
- Increasing the tone and increasing the efficiency of the entire body.
PHYSIOTHERAPY
Physiotherapy in the treatment of osteochondrosis is used, depending on the stage of the disease and the patient's condition, both in combination with drug therapy and separately.
For degenerative diseases of the spine, depending on the symptoms and the nature of the manifestations of the disease, the following types of physiotherapy are used:
UV (LOCAL ULTRAVIOLET RADIATION)
Direct exposure of the skin to UV light stimulates the production of vitamin D, which plays a key role in the absorption of calcium. The procedure is carried out using radiation, which has bactericidal, anti-inflammatory and analgesic effects.
ULTRASONIC.
Exposure of body tissues to high-frequency sound radiation (from 20 Hz). They are used in combination with various anti-inflammatory and analgesic drugs for external use to better penetrate the body tissues. The main purpose of the method is the elimination of the pain syndrome of various localizations.
SHOCK WAVE THERAPY
The essence of the procedure is the transmission of a sound wave to the pain point. The main goal is to relieve pain, improve microcirculation in the blood and speed up metabolism.
LASER THERAPY
Impact with special helium-neon lasers. Such radiation promotes the activation of bioelectrical processes in nerve tissues and has anti-inflammatory and analgesic effects. The laser is applied to the inflamed roots of the spinal nerve, which are located near the affected area of the spine.
MAGNETOTHERAPY
Exposure to the affected area of the spine to a magnetic field, which creates a bioelectric field in the tissue that stimulates all metabolic processes in the affected area at the cellular level. The magnet has anti-inflammatory and antispasmodic effects.
ELECTROPHORESIS
Expose the affected area to a weak electric shock. Under the influence of an electric field, particles of a dispersed medium can easily move in gaseous and liquid media. In this way, the necessary medication can be delivered directly to the affected area, which greatly increases the effectiveness of the treatment.
BALNEOTHERAPY
Methods of treating osteochondrosis using different types of mineral water: baths, showers, pools. During the procedure, mineral particles penetrate the skin and affect the nerve centers.
MUD
The treatment of osteochondrosis with mud is used in the form of mud applications (wraps). The influence on the body comes from the influence of high temperatures in combination with the chemical composition of the mud. In the affected tissues, the metabolism is accelerated, the blood circulation is improved, an anti-inflammatory effect is exerted and the severity of the pain syndrome decreases.
TRACTION THERAPY (BACK LENGTH)
One of the most effective treatments for osteochondrosis. During the stretching, a stretching of the muscle-ligament apparatus of the spine occurs, the distance between the vertebrae increases by 2-4 mm. Possible hernias and protrusions are reduced. Excessive pressure on the nerve roots and blood vessels, which can be hernias and osteophytes (bone growth on the vertebrae), is relieved. Spinal traction also helps reduce local edema, improve blood flow, and relieve excessive tension in the muscle-ligamentous apparatus.
VACUUM MASSAGE
The procedure is carried out with medical cups or a special device. During vacuum therapy, the blood vessels of the internal organs are stimulated. In the places where the massage was performed, the production of enzymes, biologically active substances that accelerate internal metabolism and activate regeneration processes. With continued use, the procedure can replace significant tissue rejuvenation at the application site.
CRYOTHERAPY
Sharp short-term cooling of the body to critically low temperatures, which has a therapeutic effect. It is characterized by high efficiency in suppressing pain syndrome, since a sharp drop in temperature blocks the pain receptors and significantly increases the pain threshold. It has excellent anti-inflammatory effects. There is a decrease in the level of collagenase (an enzyme that breaks down peptide bonds in all types of collagen). The formation of granulomas is blocked. The edema of soft tissues and lymph nodes is removed, the lymph flow normalizes again.
Movement Therapy - THERAPEUTIC EXERCISE FOR OSTEOCHONDROSIS
The main task of exercise therapy is to relieve and strengthen the musculo-ligamentous apparatus of the spine in order to increase the flexibility and range of motion of the vertebrae. Exercise for osteochondrosis will help improve blood circulation and increase the permeability of the tissues surrounding the spine for better permeability of nutrients.
Basic principles of physiotherapy exercises for every type of osteochondrosis
- Classes should take place in a well-ventilated place, preferably outdoors;
- Exercise should only be performed during remission if there are no symptoms;
- The clothing should be as loose as possible and not restrict movement.
- All movements should be done smoothly, and the amplitude and number of repetitions should gradually increase.
- Immediately stop training if you experience pain;
- Much depends on the breath. Try to listen to it while you practice. All stretching exercises should be done on the exhale;
- Be sure to monitor your heart rate and blood pressure. If these indicators exceed the norm, reduce the intensity of the load;
- In every wellness practice, consistency plays an important role. In order to achieve the result as quickly as possible, observe the regularity in your classes.
- “Less is better, but more often. ” Keep the exercise at a low intensity, but ideally when you can do several times a day. Try to find time for a small gym even at work.
- The exercises are selected individually. Before starting the class, be sure to consult your doctor.
WHAT TO DO IF THE TIME IS NOT ENOUGH TO PERFORM THE EXERCISES?
If you do not have enough time to do full-fledged exercises for the prevention of osteochondrosis, we offer five-minute complexes that can be performed outside the home (e. g. at work).
MANUAL THERAPY FOR OSTEOCHONDROSIS
Manual therapy is a locally dosed physical effect on the affected area of the spine and the surrounding tissue. The aim is to restore the normal function and mobility of the vertebral segments in the damaged areas.
It is considered to be one of the most effective and gentle methods of treating osteochondrosis, especially in the early stages.
The procedure usually comprises three components:
- Relaxation massage - warming up and warming up the muscles, removing excessive tone;
- Mobilization - Using relaxation techniques and stretching to relieve cramps and improve the motor properties of the musculo-ligamentous apparatus and joints. The aim is to normalize movements, improve blood circulation and restore metabolism in areas affected by osteochondrosis. Can be done in passive technique or through traction;
- Manipulation - coercive measures aimed at bringing the vertebrae back into place and restoring the normal function of the joints.
INDICATORS AND CONTRAINDICATIONS FOR MANUAL THERAPY
Manual therapy has a number of limitations that depend on the patient's condition.
Read:
- widespread osteochondrosis with large-scale lesions of the spine;
- early stages of the disease with localized lesion;
- Functional blockade of second and third degree vertebral joints;
- spinal hernia.
Contraindications:
- tumors of the spine and paravertebral structures;
- tuberculosis;
- ankylosing spondylitis;
- trauma and postoperative period;
- vertebral instability grade 3-4;
- inflammation of the spinal cord and its membranes;
- disorders of the cerebrospinal circulation;
- pronounced pain syndromes;
- tears and severe sprains of muscles and ligaments;
- dysfunction of the nerve roots;
- spinal fractures;
- and other
TREATMENT PERIOD
Depending on the characteristics of the course of the disease, the duration of treatment can be anywhere from 1-2 weeks to 2-3 months. The number of procedures depends on the characteristics of the patient and a number of related factors.
































